Journal Club #5: Appraisal Worksheet
Student Names:
Don't use plagiarized sources. Get Your Custom Essay on
research topics
Just from $13/Page
1. What was the purpose of the systematic review?
2. In your own words, summarize how the search for studies was conducted.
3. In your own words, describe how the studies to be included for analysis were selected.
4. How many studies were included in the final analysis?
5. What was the process for determining risk of bias in the studies?
6. What conclusion did the authors draw on the quality of the studies?
Journal Club #5: Exit Ticket
Student Names:
How confident are the authors that nurse-led or –collaborative interventions to increase medication adherence really work? How does this affect whether or not you would use the findings of this study to change your practice? Why?
Age and Ageing 2017; 46:
747
–
754
doi: 10.1093/ageing/afx076
Published electronically 16 May 2017
© The Author 2017. Published by Oxford University Press on behalf of the British Geriatrics Society.
All rights reserved. For permissions, please email: journals.permissions@oup.com
Nurse interventions to improve medication
adherence among discharged older adults:
a systematic review
HENK VERLOO1,4, ARNAUD CHIOLERO2,3, BLANCHE KISZIO4, THOMAS KAMPEL4, VALÉRIE SANTSCHI4,5
1School of Health sciences, HES-SO Valais — Wallis, University of Applied sciences Western Switzerland, Chémin de l’Agasse 6,
Sion, Switzerland
2IUMSP, Lausanne University Hospital, Lausanne, Switzerland
3Institute of Primary Health Care (BIHAM), University of Bern, Bern, Switzerland
4La Source, School of Nursing Sciences, University of Applied Sciences Western Switzerland, Lausanne, Switzerland
5Service of Nephrology and Hypertension, Lausanne University Hospital, Lausanne, Switzerland
Address correspondence to: H. Verloo. Tel: +41 27 606 84 24; Fax +41 27 606 84 01. Email: henk.verloo@unil.ch
Abstract
Background: discharged older adult inpatients are often prescribed numerous medications. However, they only take about
half of their medications and many stop treatments entirely. Nurse interventions could improve medication adherence
among this population.
Objective: to conduct a systematic review of trials that assessed the effects of nursing interventions to improve medication
adherence among discharged, home-dwelling and older adults.
Method: we conducted a systematic review according to the methods in the Cochrane Collaboration Handbook and
reported results according to the PRISMA statement. We searched for controlled clinical trials (CCTs) and randomised
CCTs (RCTs), published up to 8 November 2016 (using electronic databases, grey literature and hand searching), that evalu-
ated the effects of nurse interventions conducted alone or in collaboration with other health professionals to improve medi-
cation adherence among discharged older adults. Medication adherence was defined as the extent to which a patient takes
medication as prescribed.
Results: out of 1,546 records identified, 82 full-text papers were evaluated and 14 studies were included—11 RCTs and 2
CCTs. Overall, 2,028 patients were included (995 in intervention groups; 1,033 in usual-care groups). Interventions were
nurse-led in seven studies and nurse-collaborative in seven more. In nine studies, adherence was higher in the intervention
group than in the usual-care group, with the difference reaching statistical significance in eight studies. There was no sub-
stantial difference in increased medication adherence whether interventions were nurse-led or nurse-collaborative. Four of
the 14 studies were of relatively high quality.
Conclusion: nurse-led and nurse-collaborative interventions moderately improved adherence among discharged older
adults. There is a need for large, well-designed studies using highly reliable tools for measuring medication adherence.
Keywords: medication adherence, nurse intervention, nurse-led interventions, nurse-collaborative interventions, systematic review,
older people
Background
Medication adherence—defined as the extent to which
patients take medication as prescribed by their healthcare
professionals—is an important aspect of treatment efficacy,
healthcare costs and patient safety [1, 2]. Medication
adherence also implies the notion of concordance, i.e. a
process of shared decision-making between patients and
healthcare professionals [3]. According to a WHO report,
inadequate medication adherence averaged 50% among
patients with a chronic disease [4] and represented a signi-
ficant problem that led to increased morbidity and
747
mailto: henk.verloo@unil.ch
mortality, as well as increased healthcare costs [5, 6]. Many
older adults suffer from multiple chronic diseases and are
treated with numerous medications. They are, therefore, at
a high risk of poor adherence, e.g. missing doses, discontinu-
ation, alteration of schedules and doses or overuse [7]. Non-
adherence can result in worsening clinical outcomes, including
re-hospitalisation, exacerbation of chronic medical conditions
and greater healthcare costs [8, 9]. Up to 10% of hospital
readmissions have been attributed to non-adherence [6].
Several studies have demonstrated that insufficient medica-
tion adherence is common among discharged older adults [9,
10]. Older adults experienced changes in their medication regi-
men during hospitalisation [11] and in the 1st week following
hospital discharge [8]. Such changes, as well as complex treat-
ment plans, tended to decrease medication adherence and
could be a reason for a patient’s non-adherence. Older adults
may also have restarted taking medications that were discontin-
ued during hospitalisation, failed to start new medications
initiated during hospitalisation, or taken incorrect dosages [9,
12]. Moreover, medication changes are poorly communicated
to the patient at the time of discharge [13]. Older adults are at
a particularly high risk of non-adherence in the 1st days or
weeks following hospital discharge [9]. Therefore, it is import-
ant for healthcare professionals, especially community health-
care nurses, to follow-up with older adults early and frequently
to keep them adherent to therapy. Nurses are well placed to
provide and coordinate adherence-care because they are pre-
sent in the majority of healthcare settings, are in close physical
proximity to patients, and act as interfaces between patients
and physicians [14].
Previous studies have shown that interventions such as
patient education, the use of medication management tools or
electronic monitoring reminders, can help to improve medica-
tion adherence and continuity of care among older adults [15,
16]. However, few studies have evaluated the effects of inter-
ventions to improve medication adherence after hospital dis-
charge. Our systematic review focuses on the effectiveness of
nurse-led interventions to improve medication adherence in
older home-dwelling patients who are discharged from hos-
pital; a previous Cochrane review has looked at a broader
range of interventions to enhance medication adherence, in a
wide range of patient groups [16]. More specifically, there is lit-
tle evidence on the impact of nursing interventions—whether
alone or in collaboration with other health professionals—on
medication adherence among discharged older adults [9].
This systematic review aimed to determine whether
nursing interventions alone, or in collaboration with other
health professionals, were effective in improving medication
adherence among recently discharged, inpatient, home-
dwelling older adults aged 65 years old or more, when com-
pared with those receiving usual care.
Methods and materials
This systematic review was conducted according to methods
in the Cochrane Collaboration Handbook [17] and results
were reported according to the PRISMA statement [18].
Data sources and search criteria
In collaboration with a medical librarian (B.K.), a systematic
literature search was conducted for any articles published
up to 8 November 2016, using predefined search terms in
Medline via PubMed (from 1946), EMBASE (from 1947),
CINAHL (from 1937), the Cochrane Central Register of
Controlled Trials (from 1992), PsycINFO (from 1806),
Web of Science (from 1900), JBI database (from 1998),
DARE (from 1996), Tripdatabase (from 1997), the French
Public Health Database (from 1878), International
Pharmaceutical Abstracts (IPA, from 1970) and clinicaltrial.
gov (from 2008).
The syntax consisted of four search themes intersected by
the Boolean term ‘AND’. MeSH terms included age-related
terms (Aged), medication adherence-related terms (Medication
Adherence, Patient Medication Knowledge, Prescription Drug
Misuse, Polypharmacy, Drug Therapy, Medication Therapy
Management, Pharmaceutical Preparations/Administration
and Dosage), nurse-related terms (Nursing, Nursing Care,
Nurses, Nurse–Patient Relations, Models of Nursing) and
hospital-related terms (Patient Discharge, Continuity of
Patient Care, Inpatients, Hospitalisation). The search strategy
was then adapted for EMBASE, CINAHL, the Cochrane
Central Register of Controlled Trials, PsycINFO, Web of
Science, the JBI database, DARE, Tripdatabase, IPA and
clinicaltrial.gov (see Supplementary data 2, available at Age
and Ageing online).
In addition to the electronic database searches, a hand
search of the bibliographies of all relevant articles was con-
ducted, as was a search of unpublished studies using
Google Scholar, Proquest, Mednar and Worldcat, without
language restrictions. Finally, a forward citation search of
the articles selected was also conducted using Google
Scholar.
Study selection
Two authors (H.V. and B.K.) independently screened titles,
abstracts and full texts from the literature search to deter-
mine their eligibility. Full texts were eligible for review if
they were written in English, French or German. Studies
included: (i) were either randomised clinical trials (RCTs) or
controlled clinical trials (CCTs); (ii) had evaluated the effects
of nurse interventions or collaborative interventions with
other healthcare professionals on medication adherence
compared to a usual-care group and (iii) were conducted
among recently discharged (<2 weeks after discharge) older
adults (aged ≥65 years old), living at home, and taking at
least one prescribed medication for any kind of medical
condition. Outcomes were changes in medication adherence
during follow-up as measured using different methods
[1, 14], i.e. electronic monitors, prescription refills, pill
counts, medication adherence tools/questionnaires and
patient self-reporting. Disagreements between screeners
were resolved by consensus.
Nurse interventions were classified as either nurse-led
care and nurse-collaborative care, as provided by Registered
H. Verloo et al.
748
Nurses (RN). Based on the Cochrane Effective Practice
and Organisation of Care taxonomy of health systems inter-
ventions [19], we considered patient-level interventions con-
ducted by nurses (education, counselling and teaching;
reminder interventions using telephone contact, discharge
planning or medication adherence aids, e.g. electronic moni-
tors or pill dispensers; meetings with a healthcare profes-
sional in the patient’s home). These could be alone or in
collaboration with pharmacists or physicians. We also con-
sidered interventions at the healthcare-professional level
(educational meetings and distribution of educational materi-
als; educational outreach visits with feedback through medi-
cation reviews of medical records; monitoring of medication
therapy by assessment, adjustment or change of medication;
verbal or oral recommendations to pharmacists or physi-
cians; team meetings to discuss care or refer the patient to
the physician). Interventions targeting healthcare organisa-
tions, legal regulations and financial issues were excluded.
Data extraction and risk of bias in the studies
included
Two authors (H.V. and B.K.) extracted data independently,
using a specially designed and standardised data extraction
form. If necessary, any disagreements were resolved through
discussion and consultation with the co-authors (V.S. and
A.C.). The information extracted from each study included:
(i) study author, year of publication and country; (ii) study
characteristics (including study setting and design, duration of
follow-up and sample size); (iii) participants’ characteristics
(including sex, age, medication and medical conditions);
(iv) intervention characteristics (including description and fre-
quency of nursing interventions, and the healthcare profes-
sionals involved); (v) usual-care group’s characteristics; and
(vi) types of outcome measures (including medication adherence
rates or score, and self-assessment of medication adherence).
Risk of bias in the studies included
Two authors (H.V. and B.K.) independently assessed the risk
of bias for all the studies included, using the Cochrane Risk of
Bias Tool [20], a validated tool for RCTs [21–24] based on six
domains: adequate sequence randomisation, concealment of
allocation, blinding of outcome assessors, adequately addressed
incomplete outcome data, selective outcome reporting and
other risks of bias. Each domain was rated as: (i) low risk of
bias, (ii) unclear or (iii) high risk of bias. A study was con-
sidered of relatively high quality if it had adequate sequence
randomisation and a blinding of outcome assessors (i.e. low
risk of bias in both domains). Any disagreement in the quality
assessment was resolved by consensus.
Results
Results of the search strategy
In total, 1,546 records were identified using the electronic
search strategy, nine using grey literature and references
listed in selected papers, and 825 using the forward citations
search. After removal of duplicates, 1,265 records were
screened based on title and abstract, and 82 were con-
sidered potentially eligible and had their full texts evaluated.
A total of 14 studies satisfied the selection criteria and were
included (Figure 1).
Characteristics of studies and participants
The 14 studies included were conducted on three conti-
nents (Europe, n = 5; Asia, n = 2 and North America,
n = 7), in seven countries (Canada, China, Denmark, Italy,
Israel, Netherlands and the USA), and were published
between 1989 and 2015 (Table 1). Eleven studies were
RCTs and three were CCTs. Ten RCTs were randomised at
the patient level and one at the hospital level (cluster).
Overall, interventions involved nurse-led care in seven stud-
ies and nurse-collaborative care in seven more.
The 14 studies involved a total of 2,028 participants
(995 in experimental groups; 1,033 in usual-care groups)
aged from 63 to 83 years old and followed-up over a mean
of 5.3 months (SD = 4.7; range: 1–12 months). All studies
included men and women. The patient groups included
were older discharged inpatients with cardiovascular dis-
eases (n = 8), post-surgical interventions in geriatric and
internal medicine units (n = 4), chronic obstructive pulmon-
ary disease (n = 1) or stroke with hypertension (n = 1).
Characteristics of nurse interventions
All studies employed discharge planning and patient educa-
tion as usual-care activities to improve medication adher-
ence. These interventions were carried out in hospital and/
or at the participant’s home (counselling and patient educa-
tion/teaching). The interventions exclusively delivered by
RNs or implemented in collaboration with other healthcare
professionals were multidimensional. Hence, some interven-
tions integrated other healthcare professionals and patients
through meetings, education sessions or reminders (see
Supplementary data 1, available at Age and Ageing online).
The majority of the nurse-led interventions involved
comprehensive assessments of medication during home vis-
its, verbal advice, medication education and written fact-
sheets, care plans and medication schedules, and verbal and
written reminders by telephone or using electronic devices,
mostly done by nurses and by electronic pill dispensers [21,
22, 24, 25, 28, 32, 33].
The nurse-collaborative interventions were more
focused around participants’ clinic visits, integrating coun-
selling and comprehensive teaching by a pharmacist or a
physician about the importance of medication adherence,
and the aid of electronic devices such as weekly tele-
monitoring, daily ECG, weighing, medication organisers
and electronic patient reminders about medication adher-
ence [23, 26, 27, 29–31]. Two collaborative interventions
used medication adjustments by the pharmacist, organised
Nurse interventions to improve medication adherence
749
feedback to other healthcare professionals, and proposed
social and personal support [27, 30].
Medication adherence
Five studies assessed medication adherence as the primary
outcome [23, 26, 29, 32, 34] and nine studied it as a sec-
ondary outcome [21, 22, 24, 25, 27, 28, 30, 31, 33]. Pill
counts [29] were used to measure medication adherence, as
were the following standardised, validated instruments: the
Brief Medication Questionnaire (BMQ) [25, 27], the
Medication Adherence Scale [28], the Medication Error
Rating [21], the Medication Possession Rating [26, 31] and
the Modified Centre for Adherence Support Evaluation
(CASE) adherence index [39]. Self-reported measures [22,
30, 32–34] and the medication pharmacy prescription refill
[23] were used in almost half of the studies retrieved (see
Supplementary data 3, available at Age and Ageing online).
A 1-month study using pill counts was conducted by a
pharmacist visiting patients at home or during patients’
pharmacy visits [29]. Tsuyuki et al. [31] employed pharmacy
records over 6 months to calculate the Medication
Possession Ratio, documented as one of the most accurate
and reliable methods of measuring medication adherence
[35]. Barnason et al. and Eggink et al. measured medication
adherence over three and one-and-a-half months, respect-
ively, using the BMQ [36]; Garcia-Aymerich et al. employed
the Medication Adherence Scale [37] over 12 months; and
Kennedy used the Medication Error Rating Tool [38] over
1 month to discriminate between medication adherence and
non-adherence. Tsuyuki et al. [31] and Wolfe and Schirm
[32] measured medication adherence using the Medication
Possession Ratio and the Medication Rating Scale, respect-
ively. Weller employed a weekly/monthly pill dispenser and
measured medication adherence over 3 weeks using the
CASE adherence index [39]. Self-reporting was based on
Figure 1. PRISMA flow diagram summarising the results of the search strategy.
H. Verloo et al.
750
telephone calls, interviews during home visits or the analysis
of participants’ logbooks (see Supplementary data 3, available
at Age and Ageing online). Home visits varied between daily
[29], weekly [24, 30, 33], and monthly follow-up visits [22,
32], mostly made by a nurse or a pharmacist. Telephone call
follow-up and adherence reminders varied from weekly [21,
24, 25, 28, 31, 33, 34], monthly, to three-monthly contacts
[26, 27]. One study assessed participants’ weight weekly
using an electronic device [31] and Antonelli et al. assessed
weekly electrocardiograms (ECG) by tele monitoring [34].
Only four of the 14 studies reported the duration of the
interventions [22, 23, 28, 30]. Table 1 presents the nurse-led,
nurse-collaborative interventions and the details of the fre-
quency and the durations of the interventions.
Effects of nurse interventions
The diversity of measurement instruments, medical condi-
tions and the complexity of the intervention designs made
it difficult to summarise the effects of those interventions
on the improvement of medication adherence. In nine
studies, medication adherence was higher in the interven-
tion group than in the usual-care group, and the difference
reached statistical significance in eight of them. Three out
of seven nurse-led interventions [21, 28, 33] and five out of
seven collaborative-care interventions [23, 26, 29, 30, 34]
significantly improved medication adherence.
Nurse-led interventions among cardiac patients by
Zhao et al. [33], COPD patients by Garcia-Aymerich et al.
[28], and post-surgical patients by Kennedy et al. [21] were
all associated with improvements in medication adherence.
No improvements were observed in the studies conducted
among stroke patients by Hornnes et al. [22], geriatric
patients by Weller [24], or post-surgical patients by Wolf
and Schirm [32].
Nurse-collaborative interventions conducted among cardiac
patients by Antonicelli et al. [34], Bisharat et al. [26], Rich et al.
[29] and Rinfret et al. [23] were all associated with improve-
ments in medication adherence. However, nurse-collaborative
interventions among cardiac patients conducted by Eggink
et al. [27] and Tsuyuki et al. [31] were not associated with
improvements in medication adherence. In the study by
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Table 1. Characteristics of the studies included
References,
country
Design Setting Medical condition Study
duration
(months)
Type of
intervention
Usual care
Antonicelli et al.
[34], Italy
RCT Outpatient clinic
Congestive heart
failure
12 Nurse-
collaborative
intervention
Routinely planed care visits in the outpatient
clinic with a nurse
Barnason et al.
[25], USA
RCT Hospital care with
follow-up
Heart failure
3 Nurse-led
intervention
Routine discharge procedure for patients with
heart failure carried out by a nurse
Bisharat et al. [26],
Israel
CCT Hospital with transition
care programme
Chronic heart failure 9 Nurse-
collaborative
intervention
Discharge counselling by a nurse
Eggink et al. [27],
Netherlands
RCT Hospital patients at
discharge
Heart failure 1.5 Nurse-
collaborative
intervention
Routine discharge planning, including
information about drug therapy delivered
by a nurse
Garcia-Aymerich
et al. [28], Spain
RCT Hospital and home
healthcare setting
Chronic obstructive
pulmonary disease
12 Nurse-led
intervention
Standard discharge procedure for COPD
patients
Hornnes et al. [22],
Denmark
RCT Hospital and home
healthcare setting
Stroke with
hypertension
12 Nurse-led
intervention
Stroke unit’s standardised discharge routine
care
Kennedy [21],
USA
RCT Hospital and home
healthcare setting
Geriatric inpatients 1 Nurse-led
intervention
Usual discharge care and information sheet
Rich et al. [29],
USA
RCT Hospital and home
healthcare setting
Congestive heart
failure
1 Nurse-
collaborative
intervention
Conventional medical care and hospital’s
standardised discharge protocol and pre-
discharge medication instructions
Rinfret et al. [23],
Canada
RCT Hospital inpatient
follow-up at home
Drug-eluding stent
with anti-platelets
12 Nurse-
collaborative
intervention
Usual counselling before discharge
Rytter et al. [30],
Denmark
RCT Hospital and
municipality care
centres
Geriatric inpatients 3 Nurse-
collaborative
intervention
Usual care made up of a short patient
education session by a nurse prior to
hospital discharge
Tsuyuki et al. [31],
Canada
RCT Hospital discharge
follow-up
programme
Heart failure 6 Nurse-
collaborative
intervention
Usual discharge planning
Weller [24], USA CCT Hospital care with
follow-up
Geriatric inpatients 3 Nurse-led
intervention
Usual discharge medication education
Wolfe and Schirm
[32], USA
CCT Hospital and home
healthcare setting
Geriatric inpatients 1.5 Nurse-led
intervention
Usual discharge planning procedure
Zhao and Wong
[33], China
RCT Hospital transitional
care programme
Coronary heart
disease
3 Nurse-led
intervention
Routine usual-care protocol
Nurse interventions to improve medication adherence
751
Rytter et al. [30] a nurse-collaborative intervention among
post-surgical patients was associated with improvements
in medication adherence (P = 0.03).
Risk of bias and methodological quality of the
studies
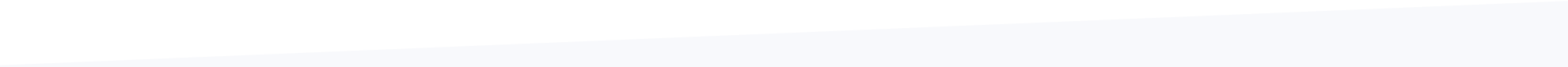
Figure 2 shows the risk of bias graph in included studies. In
most domains, few studies had a low risk of bias. Only 4 of
14 studies displayed adequate sequence randomisation and
a blinding of outcome assessors and were thus considered
of relatively high quality.
Discussion
To the best of our knowledge, this was the first systematic
review to evaluate nurse interventions aimed at improving
medication adherence among discharged older patients,
based on RCTs and CCTs. In total, 14 studies were
included, incorporating 2,028 participants. Interventions
were nurse-led in seven studies and nurse-collaborative in
seven more. In nine studies, medication adherence was
higher in the intervention group than in the usual-care
group, and this difference reached statistical significance in
eight studies. The five remaining studies showed no differ-
ence in medication adherence. However, very few studies
were of relatively high quality. We concluded that nurse-led
and nurse-collaborative interventions can improve medica-
tion adherence among discharged older adults.
This review has several limitations. One limitation was
that many of the studies failed to provide sufficient detail to
allow a precise assessment of the risk of bias, or the exact
nature, frequency and duration of the intervention tested
itself. Additionally, intervention and usual-care groups were
not always described in sufficient detail. For example,
although a study might clearly state that patients received
reminders, the means of administering them was not always
described, or was only partly described. This also raised the
issue, in many of the studies, of an adequate description of
the usual-care group. Some studies merely reported that the
participants in the usual-care group received usual care, but
did not describe what this entailed. If usual care was already
performing relatively well, then it would be harder to show
any improvement due to the intervention. Since we used
the term ‘ageing’ as a Mesh term or keyword in the search
strategy, we may have missed some relevant studies.
Another limitation was the difficulty in accurately asses-
sing medication adherence. It is well documented that stud-
ies using self-reporting by patients overestimate medication
adherence [40]. These studies are at a high risk of bias
when the participant is not blinded to the intervention. The
lack of blinding is a limitation; it is especially problematic
when adherence was estimated using questionnaires.
Indeed, patients in the intervention group may have overes-
timated their self-reported adherence. Although validated
questionnaires are available, their accuracy and reliability are
often limited and they depend on the context in which they
are used [41]. Pill count is a more objective measure, used
in some studies, and it is less exposed to bias than methods
based on self-reporting. However, most pill counts are
done using pill containers that the participant manages
alone or brings along to visits to healthcare professionals,
and in these circumstances counts can clearly be altered by
the participant [42]. Intervention components that could be
explored further include newer information and communi-
cation technologies used in addition to regular care, and the
specific or coordinated roles of allied health professionals.
The duration of intervention varies largely from one study
to the other. The association between the duration of inter-
vention and the effect on the outcome was not clear.
All the studies included were relatively small, with sample
sizes ranging from 40 to 303 participants. Relatively small
studies are more likely to miss significant differences in medi-
cation adherence, even when the intervention substantially
improves medication adherence [43]. If clinical trial studies
need hundreds or thousands of participants to show that
interventions improve medication adherence over usual care,
then it is unlikely that improving medication adherence
among older patients will have a substantial effect on major
health outcomes [43]. Innovative ideas to improve medication
adherence should be tested in much larger trials in order to
document their effects on clinically important outcomes
(including adverse effects), their feasibility in everyday practice
settings, and their sustainability.
0% 20% 40% 60% 80% 100%
No other risk of bias?
Selective outcome reporting?
Incomplete outcome data adressed?
Blinding of outcome assessors?
Allocation concealment?
Adequate sequence generation randomization?
Yes (low risk of bias) Unclear No (high risk of bias)
Figure 2. Risk-of-bias graph in included studies based on review authors’ judgments about each domain of the risk-of-bias tools.
H. Verloo et al.
752
Finally, the lack of substantial evidence could be
explained by the fact that we do not understand exactly what
medication adherence problems consist of in sufficient detail.
Frameworks to assist the development of complex interven-
tions, therefore, advise preparatory assessments involving
patients and other stakeholders, in order to better understand
the problems and the context. More objective measures of
medication adherence are needed to determine intervention
effects accurately, and investigators should make use of best-
in-class adherence measures, such as prescription monitoring.
Researchers should invariably design studies to minimise the
risk of bias and should report their procedures clearly.
Despite an extensive search, we may have missed some
trials that met all of the present study’s criteria. We identi-
fied 14 studies evaluating the effect of nurse interventions
on medication adherence among discharged older patients.
Overall, this systematic review was conducted using high
methodological standards, and it is, therefore, highly cred-
ible. However, due to the important heterogeneity between
studies (design, type of intervention) and their relatively low
quality, the level of confidence in the true effect of the
nurse interventions on medication adherence is low.
Therefore, there is still a need for large, well-designed RCTs
using highly reliable tools. Of note, non-adherence is also
of concern among younger patients, notably those with
chronic psychiatric diseases such as schizophrenia and
major depression. To the best of our knowledge, there has
been no systematic review evaluating the effects of nurse
interventions to improve medication adherence at the time
of discharge among this type of patients.
Conclusion
This systematic review examined the effects of nurse-led
and nurse-collaborative interventions to improve medica-
tion adherence among discharged home-dwelling older
adults. The complex nurse-led and nurse-collaborative inter-
ventions retained for this study tended to improve the
medication adherence to long-term medication prescrip-
tions among home-dwelling older adults. However, very
few studies were of a relatively high quality, thus limiting
our confidence in the true effect of these interventions.
There is, therefore, a need for further well-designed studies
involving large samples and using highly reliable tools, for
example, innovative e-health technologies (telephone appli-
cations) combined with pill counts to measure medication
adherence among home-dwelling older adults.
Key points
• Nurse interventions to improve medication adherence.
• Insufficient medication adherence is common among dis-
charged older adults.
• Improving medication adherence among recently dis-
charged inpatient.
Supplementary data
Supplementary data are available at Age and Ageing online.
Authors’ contributions
Study design and concept: H.V. and V.S. Writing of study
protocol: all authors. Data acquisition: H.V., B.K. and T.K.
Data analysis and interpretation: H.V., A.C., T.K. and V.S.
Article drafting: H.V. Critical revision of the article for
important intellectual content: H.V., V.S., A.C., B.K. and
T.K. Statistical analysis: A.C. and T.K. All authors revised
the article for important intellectual content and gave their
final approval for the submitted version.
Conflicts of interest
The authors declared no conflicts of interest.
Funding
No external funding was implicated in this systematic
review.
References
1. Osterberg L, Blaschke T. Adherence to medication. N Engl J
Med 2005; 353: 487–97.
2. Santschi V. Adhésion au traitement médicamenteux et suivi
électronique: une approche clinique de la prise en charge à
long terme du patient chronique dans un réseau ambulatoire
patient, pharmacien et médecin. Geneva: University of
Geneva, 2007.
3. Mullen PD. Compliance becomes concordance. Making a
change in terminology produce a change in behaviour. Br
Med J 1997; 314: 691.
4. Sabate E. Adherence to long-term therapies: evidence for
action 2003. Accessed July 11, 2005.
5. Cramer JA, Roy A, Burrell A et al. Medication compliance
and persistence: terminology and definitions. Value Health
2008; 11: 44–7.
6. Col N, Fanale JE, Kronholm P. The role of medication non-
compliance and adverse drug reactions in hospitalizations of
the elderly. Arch Intern Med 1990; 150: 841–5.
7. Kazis LE, Friedman RH. Improving medication compliance
in the elderly. Strategies for the health care provider. J Am
Geriatr Soc 1988; 36: 1161–2.
8. Mansur N, Weiss A, Hoffman A, Gruenewald T, Beloosesky
Y. Continuity and adherence to long-term drug treatment by
geriatric patients after hospital discharge: a prospective
cohort study. Drugs Aging 2008; 25: 861–70.
9. Fallis BA, Dhalla IA, Klemensberg J, Bell CM. Primary medi-
cation non-adherence after discharge from a general internal
medicine service. PLoS One 2013; 8: e61735.
10. Sergi G, De Rui M, Sarti S, Manzato E. Polypharmacy in the
elderly: can comprehensive geriatric assessment reduce
inappropriate medication use? Drugs Aging 2011; 28:
509–18.
Nurse interventions to improve medication adherence
753
11. Shelton PS, Mozingo DB, Avissar PS, Karg M, Charboneau
AL, Rich W. Measuring adherence in a community-based eld-
erly population. Consult Pharm 2012; 27: 771–81.
12. Beers MH, Sliwkowski J, Brooks J. Compliance with medica-
tion orders among the elderly after hospital discharge. Hosp
Formul 1992; 27: 720–4.
13. Witticke D, Seidling HM, Lohmann K, Send AFJ, Haefeli
WE. Opportunities to reduce medication regimen complexity:
a retrospective analysis of patients discharged from a univer-
sity hospital in Germany. Drug Saf 2013; 36: 31–41.
14. Van Camp Y, Van Rompaey B, Elseviers M. Nurse-led inter-
ventions to enhance adherence to chronic medication: sys-
tematic review and meta-analysis of randomised controlled
trials. Eur J Clin Pharmacol 2013; 69: 761–70.
15. Parker R, Frampton C, Blackwood A, Shannon A, Moore G.
An electronic medication reminder, supported by a monitor-
ing service, to improve medication compliance for elderly
people living independently. J Telemed Telecare 2012; 18:
156–8.
16. Nieuwlaat R, Wilczynski N, Navarro T et al. Interventions for
enhancing medication adherence. Cochrane Database Syst
Rev 2014; 11: CD000011.
17. Higgins J, Green S. The Cochrane Handbook for Systematic
Reviews of Interventions. Chichester, UK: John Wiley &
Sons, Ltd, 2008. Cb s, editor.
18. Moher D, Liberati A, Tetzlaff J, Altman D, Group ftP.
Preferred reporting items for systematic reviews and meta-
analyses: the PRISMA statement. Br Med J 2009; 339: b2535.
19. Cochrane Effective Practice and Organisation of Care Review
Group (CEPaOoCR). Data collection checklist (2001). http://
www.epoc.uottawa.ca/reviews.htm (January 2015, date last
accessed).
20. Higgins J, Green S. The Cochrane Handbook for Systematic
Reviews of Interventions. Chichester, UK: John Wiley &
Sons, Ltd, 2008. series Cb, editor.
21. Kennedy LM. The Effectiveness of a Self-Care Medication
Education Protocol on the Home Medication Behaviors of
Recently Hospitalized Elderly ProQuest Dissertations and
Theses. Texas University, 1990.
22. Hornnes N, Larsen K, Boysen G. Blood pressure 1 year after
stroke: the need to optimize secondary prevention. J Stroke
Cerebrovasc Dis [Internet] 2011; 20: 16–23.
23. Rinfret S, Rodés-Cabau J, Bagur R et al. Telephone contact to
improve adherence to dual antiplatelet therapy after drug-
eluting stent implantation. Heart [Internet] 2013; 99: 562–9.
http://heart.bmj.com/content/99/8/562.
24. Weller J. Comparison of Home Medication Adherence in
Adults Age 65 and Older After Completion of Standardized
Discharge Medication Education or Non-Standardized
Discharge Medication Education. Regis University, 2015.
25. Barnason S, Zimmerman L, Hertzog M, Schulz P. Pilot test-
ing of a medication self-management transition intervention
for heart failure patients. West J Nurs Res 2010; 32: 849–70.
26. Bisharat B, Hafi L, Baron-Epel O, Armaly Z, Bowirrat A.
Pharmacist counseling to cardiac patients in Israel prior to
discharge from hospital contribute to increasing patient’s
medication adherence closing gaps and improving outcomes.
J Transl Med 2012; 10: 9.
27. Eggink RN, Lenderink AW, Widdershoven JW, Bemt PM.
The effect of a clinical pharmacist discharge service on medi-
cation discrepancies in patients with heart failure. Pharm
World Sci [Internet] 2010; 32: 759–66.
28. Garcia-Aymerich J, Hernandez C, Alonso A et al. Effects of
an integrated care intervention on risk factors of COPD
readmission. Respir Med 2007; 101: 1462–9.
29. Rich MW, Gray DB, Beckham V, Wittenberg C, Luther P.
Effect of a multidisciplinary intervention on medication com-
pliance in elderly patients with congestive heart failure. Am J
Med 1996; 101: 270–6.
30. Rytter L, Jakobsen HN, Ronholt F et al. Comprehensive dis-
charge follow-up in patients’ homes by GPs and district
nurses of elderly patients. A randomized controlled trial.
Scand J Prim Health Care 2010; 28: 146–53.
31. Tsuyuki RT, Fradette M, Johnson JA et al. A multicenter dis-
ease management program for hospitalized patients with
heart failure. J Card Fail [Internet] 2004; 10: 473–80.
32. Wolfe SC, Schirm V. Medication counseling for the elderly:
effects on knowledge and compliance after hospital discharge.
Geriatr Nurs (Minneap) 1992; 13: 134–8.
33. Zhao Y, Wong FK. Effects of a postdischarge transitional
care programme for patients with coronary heart disease in
China: a randomised controlled trial. J Clin Nurs [Internet]
2009; 18: 2444–55.
34. Antonicelli R, Mazzanti I, Abbatecola AM, Parati G. Impact
of home patient telemonitoring on use of beta-blockers in
congestive heart failure. Drugs Aging 2010; 27: 801–5.
35. Christensen DB. Pharmaceutical counseling and medication
adherence monitoring: an essential component of any drug
benefit program. Med Interface 1996; 9: 76–9.
36. Svarstad BL, Chewning BA, Sleath BL, Claesson C. The brief
medication questionnaire: a tool for screening patient adher-
ence and barriers to adherence. Patient Educ Couns 1999;
37: 113–24.
37. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive
validity of a medication adherence measure in an outpatient
setting. J Clin Hypertens (Greenwich, Conn) 2008; 10: 348–54.
38. Dean B, Barber N. A validated, reliable method of scoring
the severity of medication errors. Am J Health Syst Pharm
1999; 56: 57–62.
39. Mannheimer SB, Mukherjee R, Hirschhorn LR et al. The
CASE adherence index: a novel method for measuring adher-
ence to antiretroviral therapy. AIDS Care 2006; 18: 853–61.
40. Jimmy B, Jose J. Patient medication adherence: measures in
daily practice. Oman Med J 2011; 26: 155–9.
41. Odegard PS, Carpinito G, Christensen DB. Medication adher-
ence program: adherence challenges and interventions in type 2
diabetes. J Am Pharm Assoc (2003) 2013; 53: 267–72.
42. Grymonpre RE, Didur CD, Montgomery PR, Sitar DS. Pill
count, self-report, and pharmacy claims data to measure
medication adherence in the elderly. Ann Pharmacother
1998; 32: 749–54.
43. Kline RB. Beyond Significance Testing: Statistical Reform in
the Behavorial Sciences, 2nd edition. Washington, DC, US:
American Psychological Association, 2013.
Received 25 July 2016; editorial decision 1 March 2017
H. Verloo et al.
754
http://www.epoc.uottawa.ca/reviews.htm
http://heart.bmj.com/content/99/8/562
Copyright of Age & Ageing is the property of Oxford University Press / USA and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright
holder’s express written permission. However, users may print, download, or email articles for
individual use.